Esophagogastroduodenoscopy (EGD) in Texas
What is esophagogastroduodenoscopy?
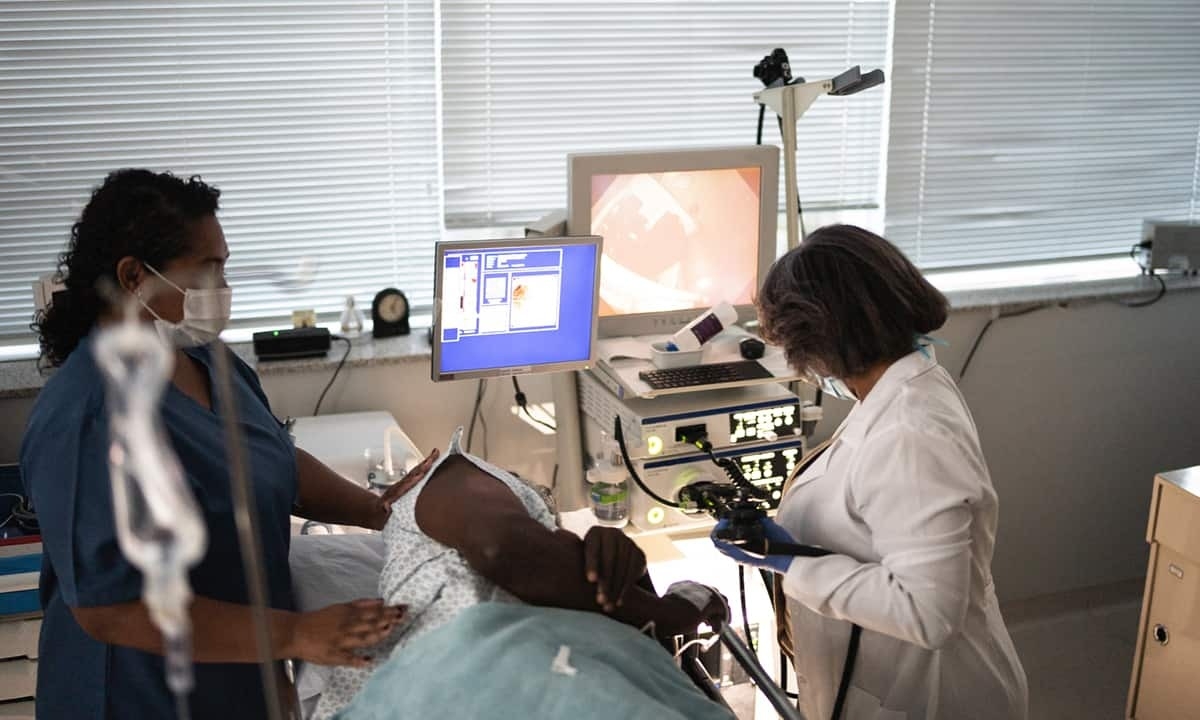
An esophagogastroduodenoscopy (EGD) is a gastrointestinal treatment in which a lengthy, skinny, malleable tube, or “scope,” is positioned into the patient’s mouth and snaked to the duodenum (where the small intestine begins). Our scope has a light and camera on the end, which helps our providers at Texas Digestive Disease Consultants to more easily inspect the lining of the esophagus, stomach, and the beginning of the small intestine.
An esophagogastroduodenoscopy is performed to discover the cause of GI issues like abdominal pain, heartburn and/or acid reflux, trouble swallowing, bleeding, or atypical x-ray results. We may also perform an EGD for Texas patients with persistent heartburn symptoms to screen for changes that might indicate esophageal cancer. If you require an EGD, please request a consultation with a skilled provider at Texas Digestive Disease Consultants.
What are the benefits of an EGD?
Having an esophagogastroduodenoscopy is often beneficial for a number of reasons. It can allow your GI physician to directly visualize the inner lining of your esophagus, stomach, and duodenum (or the first portion of the small intestine). Further benefits of an EGD are:
- Helps in detecting multiple GI conditions (including GI infections, GERD, celiac disease, Crohn’s disease, and more)
- Enables the removal of polyps, tissue biopsies, and other small procedures
- May help diagnose the causes of symptoms like nausea, vomiting, pain, and heartburn
- Typically provides a safe, quick, and efficient process
What happens the day prior to my EGD?
Your provider will give you guidelines regarding the steps needed to prepare for your EGD. Most patients will be able to eat their regular meals the day leading up to the esophagogastroduodenoscopy. We may ask you not to eat or drink anything after midnight other than medication. It is vital to follow the instructions given to you by your provider at Texas Digestive Disease Consultants. We’ll also give you specific instructions about your medications. Generally, you can take them as you normally would. This may not be the case for some circumstances, especially if you’re taking blood thinners (i.e., Coumadin®, Plavix®, warfarin, anti-inflammatories, or aspirin) or if you have diabetes. In these cases, we will provide different instructions.
What will happen on the day of the exam?
You should plan to arrive at the endoscopy center in Texas 1 – 1.5 hours prior to your procedure so you can fill out the necessary paperwork before the procedure. You will have to change into a hospital gown. An intravenous (IV) catheter will be put in your arm so we can begin the sedation process. We’ll have you connected to equipment that helps your provider to monitor your heart rate, blood pressure, pulse, electrocardiogram, breathing, and oxygen level during and after your exam.
After settling into your private exam room, we’ll have you lay on your left side on the exam table. Intravenous (IV) sedation will be started. Once you are sedated, we’ll gently insert the endoscope into your mouth. The endoscope will be strategically moved through the esophagus, stomach, and duodenum. We will inject a small amount of air through the scope into the GI tract which will help us see better. Any remaining fluid in your upper gastrointestinal tract will be suctioned out through the scope. Depending on the findings of your exam, a number of additional steps might be taken, like biopsies, the removal of polyps, and management of bleeding. Depending on the findings, the exam will take approximately 10 – 20 minutes. After your exam, you will be taken to the recovery room to be monitored as the sedation wears off.
When can I expect my exam results?
Once your exam is complete, your provider will review the findings of the procedure with you. A great deal of patients can’t remember this conversation following their exam because of the effects of the sedation. We recommend you bring a friend or family member with you to this discussion. You will also go home with a typed-up report. In many cases, we’ll provide you with biopsy results within a week.
Are there alternatives to an esophagogastroduodenoscopy?
For the most part, any alternative options will revolve around the reason for scheduling an esophagogastroduodenoscopy to begin with. Typically, an EGD is the standard treatment to check for and take care of abnormalities in the upper GI tract. However, there is an x-ray called an upper GI/barium swallow that can also evaluate your upper GI tract. Keep in mind that an upper GI/barium swallow is just a diagnosis tool, however. The treatment of any findings could necessitate an esophagogastroduodenoscopy or possibly surgery.
Are there any risks with an EGD?
In general, an EGD is a safe and reliable procedure. Generally, problems develop in fewer than 1 percent of patients. Many of these problems are not significantly dangerous. However, if an issue arises, it might require hospitalization and surgery. Before your exam, a consent form will be shared with you by the nursing staff. If you have any questions or concerns, these can be discussed with your provider prior to your EGD.
Like other tests, an esophagogastroduodenoscopy is not foolproof. There is a small, established risk that irregularities, including cancers, can be missed during your EGD. It’s crucial to keep up with your GI specialists and let them know of any recent or incessant problems.
