Endoscopic Retrograde Cholangiopancreatography (ERCP) in Texas
What is an ERCP?
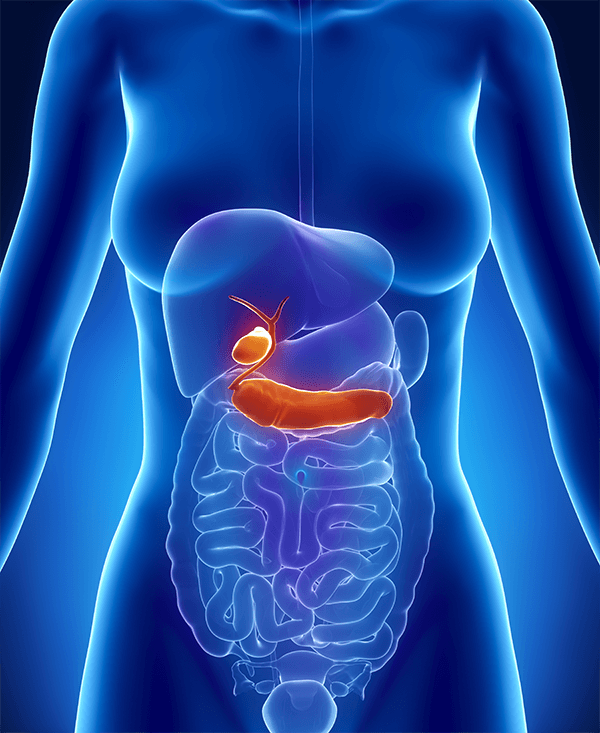
Texas Digestive Disease Consultants performs endoscopic processes to assess various types of gastrointestinal diseases and conditions in patients. An ERCP, or endoscopic retrograde cholangiopancreatography, is an endoscopic procedure in which a flexible, thin “scope” or tube is placed into the mouth and gently moved to the duodenum or first portion of the small intestine. The tube contains a camera and a light on the end of it that permits the medical provider to view the lining of the esophagus, stomach, small intestine, the opening to the bile duct, and the pancreatic duct. An endoscopic retrograde cholangiopancreatography assessment may be needed to identify the reason for several gastrointestinal concerns, including:
- Pain in the abdominal area
- Abnormal liver test
- Abnormal x-ray results
- Pancreatitis
Contact us today and request a consultation with one of our skilled providers to hear further details surrounding ERCP procedures in Texas.
What are the benefits of an ERCP?
An ERCP procedure may be recommended if blood tests show abnormal liver results, if you’re experiencing pancreatic inflammation, or if you experience symptoms such as abdominal pain or yellowing of the skin and eyes. Some benefits of an ERCP procedure are:
- Diagnostic and therapeutic: An ERCP serves dual objectives, helping doctors diagnose conditions or diseases and deliver treatment within the same procedure. This can lessen the need to undergo multiple treatment processes.
- Reduced recovery periods: Individuals commonly have faster recovery periods with an ERCP compared to conventional surgical approaches, enabling an expedited return to daily activities.
- Enhanced precision: An ERCP allows for the direct treatment and visualization of the pancreatic and biliary ducts. This is crucial for precision diagnosis and treatment.
- Efficiency: The ability to identify and treat a condition during one procedure often minimizes the total treatment time for patients.
What can I expect leading up to my ERCP exam?
Prior to your ERCP, you will be given instructions from your local Texas Digestive Disease Consultants team concerning how to prepare and what to expect. In most cases, you will be allowed to eat normally the day prior to the exam. You will be advised not to eat or drink anything after midnight except for any medications. It is essential to follow the directions administered by your physician. Further information surrounding your medications may be given. In most circumstances, your medication regimen will be followed as normal. However, in certain cases, especially in those on blood thinners (e.g., anti-inflammatories, aspirin, Coumadin®, Plavix®, and warfarin) and in diabetics, special instructions will be provided.
What can I expect during the ERCP procedure?
Your provider will ask you to show up at the endoscopy center in Texas 1 – 1.5 hours prior to your ERCP exam. This will allow adequate time to fill out paperwork and prepare for the exam. You will then need to put on a medical gown. Our clinical team will place an intravenous (IV) line in your arm to prepare for sedation to be administered. You will be connected to equipment that will enable our team to monitor your heart rate, blood pressure, pulse, electrocardiogram, breathing, and oxygen levels throughout the course of and after the procedure.
Upon entering the exam room, you will lie down on your abdomen on the table. The IV sedation will be started. Doses will be administered a little bit at a time to help make certain that you do not have an adverse reaction to the medication and that you receive only the amount you need. In comparison with other endoscopic procedures, it is not uncommon for general anesthesia to be administered for an ERCP procedure. Once you are properly sedated, the endoscope will be carefully placed into your mouth. The flexible device will be gently advanced through the esophagus, stomach, and small intestine to the location where the pancreatic and bile ducts empty into the small bowel. A small amount of air will be administered through the endoscope into the gastrointestinal tract to help the provider see. With an ERCP, an iodine-based contrast dye is injected into the bile duct and the pancreatic duct. An x-ray machine is utilized to take pictures of the biliary and pancreatic ducts to identify whether there are any abnormalities. Any residual fluid in the upper GI structures can be suctioned out by way of the scope device. Based on what the procedure reveals, a range of next steps may be taken during the course of the evaluation, including tissue biopsies, sphincterotomy (opening the bile duct or pancreatic duct), removal of gallstones from the bile ducts or stones from the pancreatic ducts, or placement of stents (plastic/metal tubes) into the bile duct or pancreatic duct. At the end of the ERCP, as much of the remaining fluid and air as possible will be removed through the endoscope tool. In general, the evaluation takes about 30 – 90 minutes based on the results.
When the procedure has concluded, you will be moved to the post-treatment room to be monitored while the sedative effects of the medication start to fade. The amount of sedation provided during the ERCP procedure and how you respond to it will impact how fast you awaken, although most people are alert enough for dismissal within 45 – 60 minutes. You cannot drive for the rest of the day and should make arrangements to have a relative or friend drive you home. You will also be advised not to perform strenuous activities, work, or sign important documents for the rest of the day. In most cases, people can resume eating and drinking as usual after being dismissed from the endoscopy unit, but specific instructions surrounding medications, activity, and eating will be given prior to discharge. Sometimes, ERCP patients might need to stay in the hospital overnight for monitoring or assessment.
When will I get my ERCP results?
Once the ERCP is complete, your provider will go over the conclusions of the procedure with you. Generally, patients will not remember what they are told following the assessment as a result of the effects of the sedation. Our Texas Digestive Disease Consultants team recommends that you bring someone with you to whom the results can also be provided. You will also be given a typed synopsis and will be advised of any biopsy or other test results often within one week.
Are there any risks associated with an ERCP?
ERCP, in general, is regarded as a very safe examination method. The majority of complications that may occur are not life-threatening, However, in the event a complication arises, it may require the need for surgery and hospitalization. Before beginning the procedure, a consent to treat form will be reviewed and discussed with the patient by the nursing team. Treatment risks will once again be explained by the doctor before the ERCP procedure gets underway, and any concerns or questions can be addressed.
A condition known as acute pancreatitis, or inflammation of the pancreas, is the most common complication. This condition may develop in 5 – 8% of individuals, but depending on the patient, the risk can be as high as 20%. Pancreatitis signs and symptoms may include nausea, vomiting, pain in the abdominal area, and fever. Most cases of pancreatitis are mild and require hospitalization for four days or less. During the hospital stay, patients commonly only require pain and nausea control along with IV fluids. A small percentage of the time, however, pancreatitis can be more severe and life-threatening.
Medication reactions related to the sedative can occur. These reactions can include but are not limited to, irritation of the blood vessel used for the IV, effects on the heart and blood pressure, allergic reactions, and breathing difficulties. Bleeding may also occur as a result of a sphincterotomy or biopsy. Major bleeding, like that which might necessitate a hospital visit or a blood transfusion, is not common.
Perforation or piercing of the small intestine, stomach, or esophagus can occur. Such an occurrence might not be identified at the time of the ERCP procedure, or it might not be evident until later in the day. In most cases, a puncture of this type will lead to hospitalization and surgery. It is important to note that this is a highly uncommon complication, even when a biopsy or sphincterotomy is performed.
For 5 – 10 percent of people, the endoscopic retrograde cholangiopancreatography assessment might not be able to be completed for several reasons. It is extremely critical that the patient reach out to the doctor’s office immediately should any type of symptoms occur following the test, such as bleeding, fever, or increasing abdominal pain.
Similar to any other test, endoscopic retrograde cholangiopancreatography is not without flaws. There is a minor, accepted risk that diseases, including malignancies, may go undetected at the time of the procedure. It is critical to regularly visit your medical practitioners as instructed and let them know of any new or ongoing symptoms or concerns.
Should you find yourself needing an ERCP in Texas, our gastroenterologists at Texas Digestive Disease Consultants can help you determine the optimal approach for you.
Are there any alternatives to an ERCP?
To some extent, any alternatives to the ERCP procedure will be based on the underlying reason for needing the endoscopic retrograde cholangiopancreatography to begin with. For the majority of patients, the ERCP process is the top approach to assess and address certain issues in the pancreatic and biliary structures. However, an x-ray referred to as a magnetic resonance cholangiopancreatography (MRCP), percutaneous transhepatic cholangiogram (PTC), echo-endoscopy or endoscopic ultrasound (EUS) can also assess the biliary ducts and pancreatic ducts. Please note that a magnetic resonance cholangiopancreatography is only a diagnostic exam. Treatment of abnormalities will involve an ERCP or a surgical procedure. In addition, EUS or PTC do have treatment alternatives. Your provider at Texas Digestive Disease Consultants will work with you to decide the best way to proceed with your specific needs.
ERCP FAQs
What are some questions to ask your physician about the ERCP procedure?
If you discover that you need an ERCP procedure, you will likely have several questions and may be unsure of where to start. Questions to consider asking your physician include:
- What does your provider anticipate finding during this procedure?
- What is the overall success rate of an ERCP?
- If a complication should arise, what signs or symptoms might you experience?
What should you avoid doing after having an ERCP?
You should not drive for 24 hours after having an ERCP procedure as the anesthesia may take that long to fully leave your body. As such, it is important to have a friend or family member take you home. You may be instructed to avoid eating for a certain timeframe depending on the type of treatment conducted during your ERCP. We also recommend that you take the rest of the day and potentially the following day off work to recover. Our Texas Digestive Disease Consultants team will help you understand what to anticipate throughout the course of the ERCP procedure.
What types of procedures can be performed during an ERCP?
Some of the more common procedures conducted during the course of the ERCP process include:
- Biliary sphincterotomy
- Removal of stones (bilestones)
- Biopsies (tissue sampling)
- Stent placement
How should you prepare for an ERCP?
Our Texas gastroenterology team will provide you with information on preparing for an ERCP procedure. However, a few instructions you’ll most likely be advised to follow include:
- Do not eat or drink for eight hours prior to your procedure. (Water may be fine. Consult your provider to confirm.)
- Do not smoke for eight hours before your ERCP appointment.
- Give your GI physician a list of any medications you take in addition to any known allergies you may have.
